Introduction
Chronic myelomonocytic leukemia (CMML) is a challenging malignancy that shares characteristics with myelodysplastic syndromes and myeloproliferative neoplasms. Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is the only curative option for CMML. Numerous studies have examined transplant outcomes and prognostic factors; however, the focus has primarily been on bone marrow transplantation (BMT) and peripheral blood stem cell transplantation, while cord blood transplantation (CBT) is understudied. To address this knowledge gap, we conducted a nationwide retrospective study to comprehensively compare the outcomes of unrelated BMT and single-unit umbilical CBT in patients with CMML.
Methods
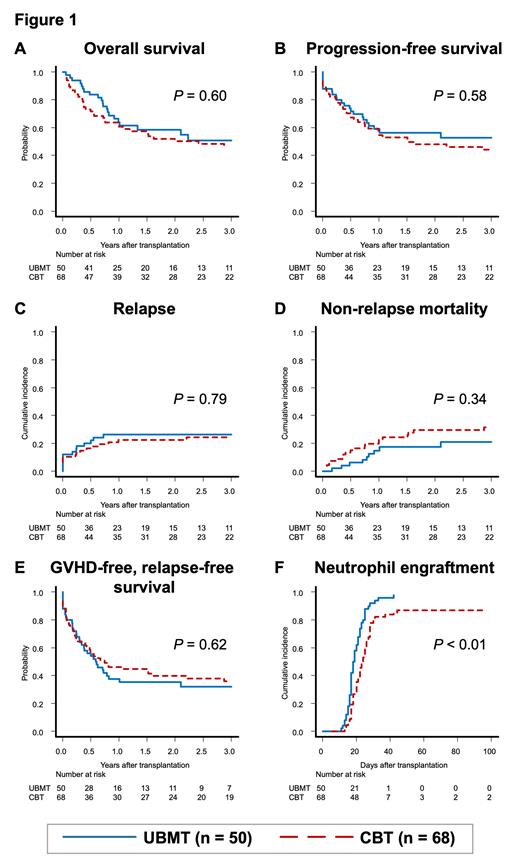
Data were collected from the Transplant Registry Unified Management Program 2 of the Japanese Data Center for Hematopoietic Cell Transplantation. The inclusion criteria were as follows: age of 16 years or higher, a diagnosis of CMML, and receipt of the first allo-HSCT between 2013 and 2019 through unrelated BMT from a human leukocyte antigen (HLA) 8/8-matched donor (UBMT group) or single-unit umbilical CBT (CBT group). The primary endpoint was overall survival (OS) after allo-HSCT, and the secondary endpoints included progression-free survival (PFS), cumulative incidences of relapse and non-relapse mortality (NRM), neutrophil engraftment, and graft-versus-host (GVHD)-free, relapse-free survival (GRFS).
The impact of CBT versus unrelated BMT on outcomes was evaluated using inverse probability of treatment weighting (IPTW) analysis. In this analysis, the Cox proportional hazards regression model for OS, PFS, and GRFS and the Fine-Gray proportional hazards regression model for relapse, NRM, engraftment, and GVHD were used. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated for all outcomes. The propensity score (PS) was calculated via logistic regression by using the following factors: age at allo-HSCT, sex, cytogenetic risk, disease status, days from diagnosis to allo-HSCT, and year of allo-HSCT. For the CBT group, the stabilized weights were calculated by dividing CBT prevalence by each individual's PS. Conversely, for the UBMT group, the weights were calculated by dividing the 1 minus prevalence of CBT by 1 minus each individual's PS.
Results
Between 2013 and 2021, 238 patients with CMML underwent their first allo-HSCT. Among them, 50 underwent HLA 8/8 allele-matched unrelated BMT (UBMT group) and 68 underwent single-unit umbilical CBT (CBT group). The median age at allo-HSCT was 58.5 (range: 26-75) years; the median follow-up period for survivors was 1,329.5 (range: 100-1,967) days. Intergroup differences in age at allo-HSCT, recipient sex, hematopoietic cell transplantation-specific comorbidity index, Eastern Cooperative Oncology Group performance status, cytogenetic risk, pre-transplant treatment, disease status at allo-HSCT, conditioning intensity, GVHD prophylaxis, and year of allo-HSCT were not significant.
The transplantation outcomes are shown in Figure 1. There were no significant differences in the 3-year OS rate (UBMT: 51.0% [95% CI: 34.1-65.5%] vs CBT: 46.2% [95% CI: 33.2-58.1%]; P = 0.60; Figure 1A). IPTW analysis revealed no significant differences between the CBT and UBMT groups (HR: 1.21, 95% CI: 0.69-2.10, P = 0.51). PFS, relapse, NRM, and GRFS were not significantly different between the groups (Figure 1B-E). The neutrophil engraftment rate at 30 days was significantly higher in the UBMT group than in the CBT group (UBMT: 92.0% [95% CI: 78.9-97.1%] vs CBT: 79.4% [95% CI: 67.5-87.4%]; P < 0.01; Figure 1F). These observations associated with the secondary endpoints were concurrently corroborated by the IPTW analysis.
Conclusion
Our study suggests that CBT can serve as a viable treatment option, demonstrating efficacy comparable to that of unrelated BMT for patients with CMML. These findings underscore the improved outcomes over time after CBT in patients with CMML, which is a treatment previously perceived as inferior to other donor sources (Itonaga et al., Biol Blood Marrow Transplant. 2018;24:840-48). Further investigations are warranted to optimize transplantation strategies and improve outcomes in patients with CMML.
Disclosures
Doki:Novartis Pharma K.K.: Honoraria; Janssen Pharmaceutical K.K.: Honoraria. Tanaka:Pifzer: Speakers Bureau; Sumitomo Pharma: Speakers Bureau; abbvie: Speakers Bureau; Asahi Kasei Pharma: Speakers Bureau; CHUGAI PHARMACEUTICAL CO., LTD.: Research Funding, Speakers Bureau; DAIICHI SANKYO COMPANY, LIMITED: Speakers Bureau; Kyowa Kirin: Speakers Bureau; MSD: Speakers Bureau; Otsuka Pharmaceutical: Speakers Bureau. Takahashi:Nippon Sinyaku: Honoraria; Daiichi Sankyo RD Novare, Otsuka Pharmaceutical: Research Funding; Novartis: Honoraria; Chugai Pharmaceutical: Honoraria; Asahi Kasei Pharma: Honoraria; AstraZeneca: Honoraria; Terumo: Honoraria; Kyowa Kirin: Honoraria; JCR pharma: Honoraria. Ozeki:AbbVie GK: Honoraria; Takeda Pharmaceuticals: Honoraria; Janssen Pharmaceutical K.K.: Honoraria; Asahi Kasei America, Inc.: Honoraria; CHUGAI PHARMACEUTICAL CO., LTD.: Honoraria; Sanofi K.K.: Honoraria. Nakamae:Alexion: Other: Project funding; Takeda Pharmaceuticals: Other: Project funding; Novartis Pharmaceuticals: Other: Project funding; Parexel International Inc.: Other: Project funding; CMIC CO.,Ltd.: Other: Project funding; Janssen Pharmaceutical K.K.: Honoraria; DAIICHI SANKYO COMPANY, LIMITED: Honoraria; Bristol Myers Squibb: Research Funding; Astellas Pharma Inc.: Honoraria; AbbVie GK: Honoraria; Amgen K.K.: Honoraria; Otsuka Pharmaceutical: Honoraria; Sumitomo Dainippon Pharma Co., Ltd.: Honoraria; Nippon Shinyaku Co., Ltd.: Honoraria; Bristol Myers Squibb: Honoraria; Meiji Seika Pharma Co., Ltd.: Other: Project funding. Kanda:Precision: Speakers Bureau; AbbVie: Research Funding, Speakers Bureau; CSL Behring: Speakers Bureau; Japan Blood Products Organization: Research Funding, Speakers Bureau; Otsuka Pharmaceutical: Research Funding, Speakers Bureau; AstraZeneca: Speakers Bureau; Human Life CORD: Speakers Bureau; Sumitomo Pharma: Research Funding, Speakers Bureau; Amgen: Speakers Bureau; Takeda Pharmaceutical: Research Funding, Speakers Bureau; Meiji Seika Pharma: Speakers Bureau; Asahi Kasei Pharma: Research Funding, Speakers Bureau; Daiichi Sankyo: Research Funding, Speakers Bureau; Saitama Hokeni Kyokai: Speakers Bureau; MSD: Speakers Bureau; Kyowa Kirin: Research Funding, Speakers Bureau; Janssen Pharmaceutical: Speakers Bureau; Sanofi: Speakers Bureau; Pfizer: Speakers Bureau; Chugai Pharmaceutical: Research Funding, Speakers Bureau; Novartis: Speakers Bureau; Bristol Myers Squibb: Speakers Bureau; Towa Pharma: Speakers Bureau; FUJIFILM Wako Pure Chemical: Speakers Bureau; Shionogi Pharma: Research Funding; Alexion Pharma: Speakers Bureau; Eisai: Research Funding, Speakers Bureau; Nippon Shinyaku: Speakers Bureau; Wakunaga Pharmaceutical: Speakers Bureau; Taiho Pharmaceutical: Research Funding; Nippon Kayaku: Research Funding; JCR Pharmaceuticals: Research Funding. Atsuta:JCR Pharmaceuticals Co., Ltd.: Consultancy; Otsuka Pharmaceutical Co., Ltd: Speakers Bureau; Novartis Pharma KK: Speakers Bureau; CHUGAI PHARMACEUTICAL CO., LTD.: Speakers Bureau; Meiji Seika Pharma Co, Ltd.: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal